Does the average health plan member pay thousands in premiums every year just to feel like a number? Or do they feel like someone has their back, helping them improve their health, save money, and simplify a complex healthcare system?
As consumers, we all know which we’d prefer.
New transparency rules from the Centers for Medicare and Medicaid Services (CMS) could make that experience more common, or at least one that resembles the way consumers shop for everything else in life. Much will depend on how plans embrace the new requirements (or get around them) over the next few years.
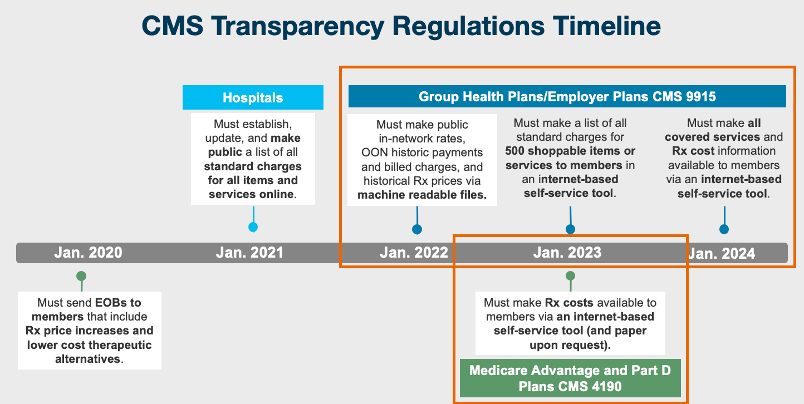
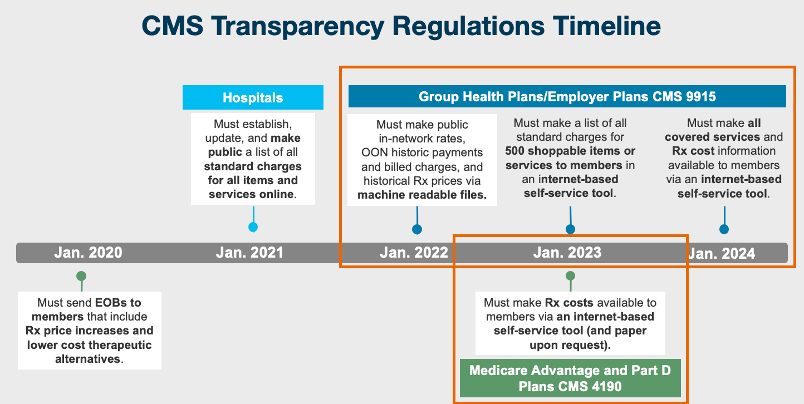
Rather than simply comply, plans can use CMS transparency rules as an opportunity to better educate members about covered services and medications, clearly display accurate costs, and make the information easy to find. If our experience in drug price transparency is any guide, member engagement and satisfaction are natural byproducts.
At Rx Savings Solutions, we’ve always believed transparency and simplicity lead to engagement.
The pandemic has amplified the need for a member experience that will overcome barriers and get members to close critical gaps in care, like scheduling a screening or filling important medications. Our partnership with Welltok accelerates this goal, driving a better member experience with their unique recipe for consumer activation. It’s a combination of data, analytics and multi-channel motivation that creates a chain reaction, one that leads to more satisfying healthcare experiences.
Both companies can attest that done the right way, transparency builds trust.
Helping Members Understand their Benefits
If we’re honest about it, most people choose a health plan option based on whatever premium their budget can handle. Few understand the impact of higher deductibles and co-insurance on their total cost of care and medications. That’s a good reason for plans to help members optimize their medical and prescription drug benefits. The more clarity and less guesswork members have, the fewer unpleasant surprises they encounter—like a $500 prescription that used to cost them $5 under a previous plan option.
If their health plan can proactively notify them of that reality and point them to a lower-cost therapy, unnecessary costs aren’t the only things avoided. Think about sticker-shock at the pharmacy and the resulting ill will toward the plan—not to mention the downstream consequences of skipping or rationing the medication.
An optimized benefit experience will create more of a two-way relationship, a valuable interaction between your plan and an individual member. It’s exactly the experience Rx Savings Solutions, Welltok and other healthcare solution providers strive for, along with the lasting engagement it can create.
“Engaging with health benefits or anything else requires a personal connection, even when technology is the primary conduit,” said John Coleman, Welltok’s Associate Vice President of Market Solutions. “Offering our health plan clients the opportunity to provide a cost transparency tool like Rx Savings Solutions helps drive an overall better member experience while increasing medication adherence. Access to affordable medication also enhances total wellbeing and ultimately helps organizations meet their quality and revenue goals.”
Rinse, Repeat, Engage
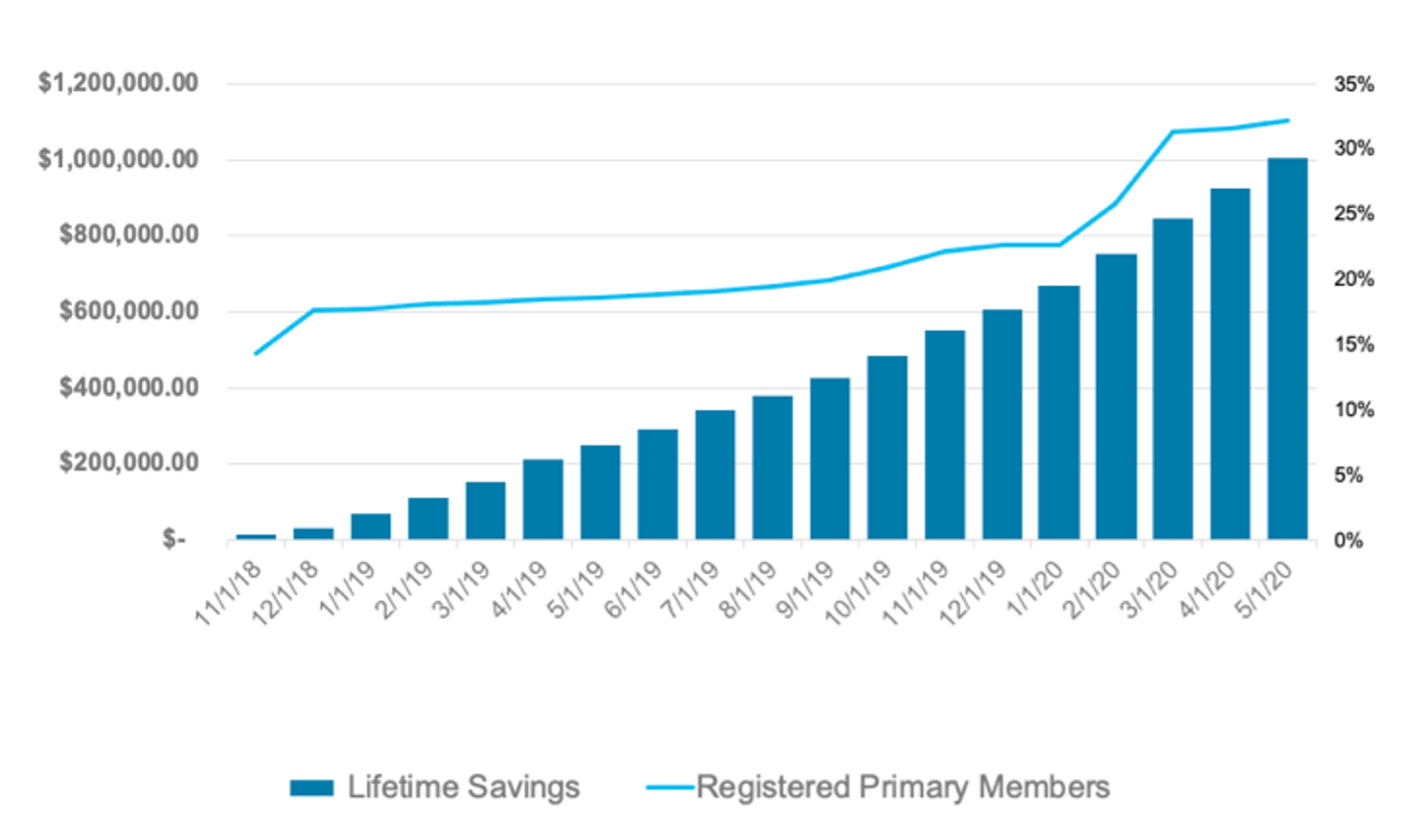
A more transparent approach can change the experience—from feeling like a number to feeling cared for—one member at a time, times millions. Common sense and experience tell us that repeated positive interactions—whether with people, products or providers—build loyalty and ongoing engagement. We see this happen over time with our own solution. Engagement builds on itself. So do cost savings.
The right transparency and advocacy tools can deliver the same win-win for health plans across the spectrum of care. That won’t happen overnight, but plans can accelerate the shift by embracing transparency with a relationship-minded, member-first approach.
Engagement/savings growth, months 1-18; employer-sponsored plan with 38,500 RxSS-eligible members:
———————————————————-
STAY UP TO DATE
Sign up for our monthly newsletter, The Script, and we’ll send you a quick run-down of industry updates, thought leadership and our latest insightful blogs to keep you informed.



